A Comprehensive Guide to Hysterectomy Procedures
September 2, 2024
Understanding Hysteroscopy and Related Procedures: What You Need to Know
October 23, 2024
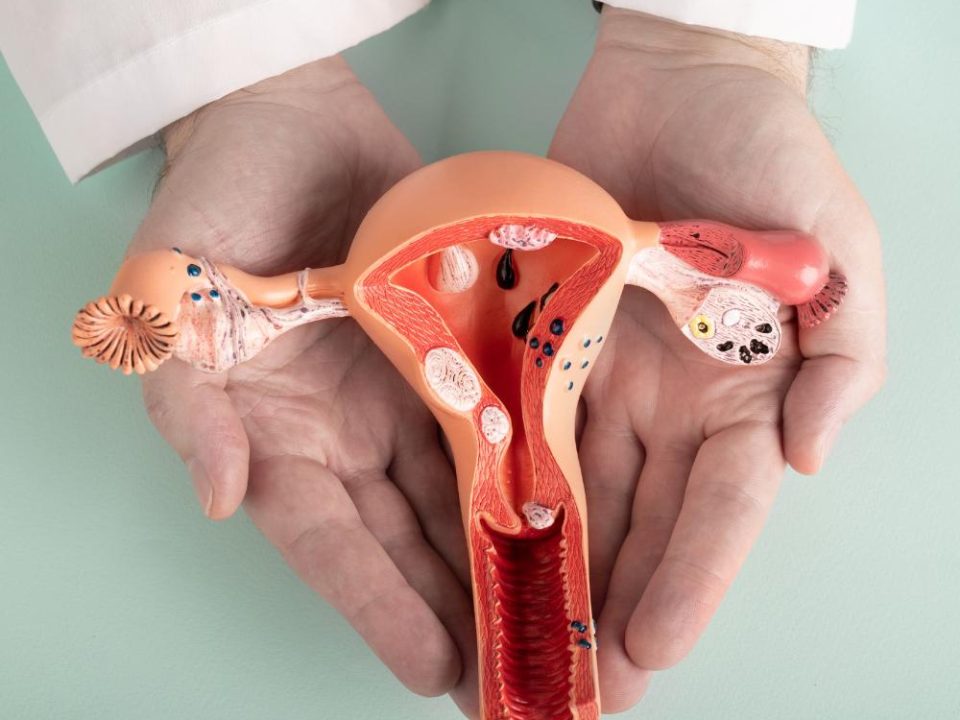
Chronic Pelvic Pain (CPP) is a prevalent medical condition affecting over 1 in 10 women in the United States. It is defined as pelvic pain that persists for more than six months, often continuing even after the initial cause has resolved. Women with CPP often experience limitations in daily activities, pain during intercourse, and symptoms of depression.
Understanding Acute vs. Chronic Pain
Acute pain is short-term and typically linked to an immediate cause, while chronic pain lasts for an extended period, leading to physical, emotional, and behavioral changes.
Chronic Pelvic Pain Syndrome involves:
Pain lasting 6+ months.
Limited relief from conventional treatments.
Pain intensity beyond the initial injury.
Depression symptoms, such as trouble sleeping, changes in appetite, and decreased physical activity.
CPP and Other Body Systems
Long-term CPP can impact other muscles and organs, causing muscle tension that affects the bladder, bowel, back, and legs. This pain can spread due to nerve interactions and muscle changes, requiring doctors to examine all organ systems for an accurate diagnosis.
How Pain is perceived
Pain signals travel through the nervous system to the brain, where they are processed. Chronic pain can alter how the central nervous system interprets these signals, making the pain persist even after the original injury has healed.
Factors Contributing to Chronic Pain
Pathology at the Site of Origin: Initial injury or condition (e.g., endometriosis or cysts) that caused the pain.
Referred Pain: Nerves from different organs and muscles overlap, spreading the pain.
Trigger Points: Areas of muscle tenderness that may become a primary pain source.
Brain Action: Emotional states, like depression, can increase pain perception.
Treatment Approach
Effective CPP treatment involves addressing all factors—physical, emotional, and behavioral. A combination of therapies may include:
Physical therapy for muscle and posture evaluation.
Psychological counseling for emotional support.
Medications to manage pain.
Factors Doctors Consider
Doctors evaluate all contributing factors since CPP usually results from multiple interacting causes. A comprehensive, multi-treatment approach is essential, and it may take weeks or months to notice improvement.
Musculoskeletal and Emotional Treatment
Physical therapy may include exercises, relaxation techniques, and use of specialized equipment. Emotional support is also vital, involving therapy to manage depression, anxiety, and the impact on relationships.
Surgical Options
In some cases, surgery (e.g., hysterectomy or scar tissue removal) may be considered but is not always effective for CPP. A hysterectomy, for example, does not guarantee pain relief and carries risks, so it should only be pursued after other treatments.
Realistic Expectations for Treatment
Treatment may not fully eliminate CPP, and results can take time. Doctors aim to reduce pain and improve quality of life, helping women manage their roles as wives, mothers, and professionals with minimal discomfort. Chronic pain management is a gradual process, requiring patience and adherence to a comprehensive treatment plan.
Medication and Pain Management
Patients should follow up with their primary care physicians for long-term pain management, as consultative clinics typically coordinate care rather than provide ongoing narcotic prescriptions. Treatment may involve various specialists to address the different aspects of CPP, ensuring a holistic approach.